As many as 75% of children undergoing surgery experience significant preoperative anxiety and fear (Getahun et al., 2020; Liang et al., 2021). Preoperative anxiety is linked to regressive postoperative behaviors (Batuman et al., 2016; Kain et al., 2006) experienced by over 75% of children undergoing surgery (Lao et al., 2020). Before a child’s surgery, parents also display high levels of anxiety, which is strongly correlated with child anxiety (Getahun et al., 2020; Liu et al., 2022). Psychological preparation before surgery, particularly when provided by a child life specialist (Brewer et al., 2006), is believed to prevent many physiological and behavioral concerns associated with anxiety (Kain et al., 2007).
Research into which preparation techniques are most beneficial is limited and warrants further study. No standard of preparation technique exists, although there is some evidence for the use of specific approaches. Informational videos based on modeling reduce anxiety at time of anesthesia induction, as well as negative post-surgery behavioral changes (Batuman et al., 2016).
The current study, a double-blind, pretest-posttest randomized controlled trial provides insight into the impact of a particular preparation technique (video modeling) on preoperative anxiety and postoperative behavior changes in children ages 5 to 10 years old. Study findings inform how preoperative preparation for children should be undertaken by healthcare providers. The research questions for the study include:
-
Does a psychological preparation video intervention impact preoperative anxiety in children ages 5 to 10 undergoing outpatient surgery?
-
Does a psychological preparation video intervention impact post-hospital behavior changes in children ages 5 to 10 undergoing outpatient surgery?
-
Does a psychological preparation video intervention impact preoperative anxiety in parents/guardians of pediatric patients undergoing outpatient surgery?
Literature Review
Short- and long-term effects of stressful healthcare encounters for pediatric patients include regression, separation anxiety, nightmares, increased fear (Rennick et al., 2004), eating problems, enuresis (Batuman et al., 2016; Rennick et al., 2004) and sleeping disorders (Kain et al., 2006). These negative psychological sequelae following a healthcare encounter have been associated with anxiety preceding the event (Batuman et al., 2016; Kain et al., 2006, 2007). In an effort to mitigate undesired outcomes, preoperative programs in children’s hospitals help ease anxiety before surgery (Batuman et al., 2016; Brewer et al., 2006; Kain et al., 2006, 2007). Providing parents with preparatory information has also been shown to reduce parental preoperative anxiety (Afzal et al., 2022; McEwen et al., 2007).
Children’s Reactions to Healthcare Experiences
Children who undergo surgery and their parents are at risk of developing traumatic stress reactions, with one study finding that over one-fourth of pediatric surgery patients experienced traumatic stress symptoms when assessed three to five months after discharge (Ari et al., 2019). Additionally, in a study by Ari and colleagues (2019), 11.6% of parents of pediatric surgery patients developed Post-Traumatic Stress Disorder. Studies of pediatric surgery patients have explored factors that increase a child’s risk for negative outcomes.
Certain demographic characteristics may increase the likelihood of preoperative anxiety in children. Quiles and colleagues (2000) found a higher incidence of preoperative worry among female patients. Additionally, pre-surgery worries increased with age. As cognition develops, children become more aware of the risks of surgery (Quiles et al., 2000). In contrast, other studies have found an inverse relationship between age and preoperative anxiety (Getahun et al., 2020; Liu et al., 2022). It may be that the source of anxiety differs by age, with older children showing concern for different factors than younger patients (Liu et al., 2022). Preoperative anxiety has also been linked to negative postoperative behavior changes (Batuman et al., 2016; Kain et al., 2006).
Cultural variables may also influence parental report of children’s postoperative behaviors. A study of pediatric outpatient surgery patients that used the post-hospital behavior questionnaire (PHBQ) found that, even after controlling for socioeconomic variables, Spanish-speaking Hispanic parents reported lower PHBQ scores than either English-speaking White or Hispanic parents (Fortier et al., 2012). The current study analyzed the relationship of demographic variables to both preoperative anxiety and postoperative behaviors and explored the interaction of the impact of the video modeling intervention with patient age, sex, language, and previous surgical history.
Various interventions have been shown to mitigate the negative impact of stressful healthcare experiences on children and families. At many healthcare facilities, child life specialist services are offered with the goal of reducing anxiety and enhancing coping (ACLP, n.d.).
Child Life Services and Psychological Preparation
Child life programs have become an integral aspect of children’s hospitals (Romito et al., 2021). Child life specialists are healthcare practitioners trained in child development who provide psychosocial care to children and families (ACLP, n.d.). A key component of child life services is psychological preparation for stressful experiences such as medical procedures.
Preoperative preparation of children reduces negative responses to healthcare experiences (Batuman et al., 2016; Brewer et al., 2006). Different methods to prepare children for medical procedures have been found beneficial. Video preparation is one effective tool to reduce anxiety (Fortier et al., 2012, 2015; Kain et Al., 2004; Kerimoglu et al., 2013; Lee et al., 2012). Modeling techniques allow children to indirectly role-play their procedures using tools such as video presentation (McCann and Kain, 2001). Batuman and colleagues (2016) examined whether an informational video including a child modeling the surgery process influenced children’s preoperative anxiety and postoperative behaviors. Video preparation was found to reduce anxiety at the time of anesthesia induction and post-hospital behaviors one week after surgery.
Brewer and colleagues (2006) conducted a double-blind study to determine if surgery patients prepared by a child life specialist demonstrated less anxiety than those who did not receive preparation. Children receiving preparation from a child life specialist had less anxiety than the control group. Furthermore, children in the control group experienced a significant increase in anxiety levels from the preoperative to postoperative period whereas the intervention group had a nonsignificant decrease in anxiety.
Method
This study was conducted in an outpatient medical center in southern California that is part of a national hospital system. A video was created by the child life specialist at this facility to prepare children for what to expect the day of surgery. Following the study design of Batuman et al. (2016), the effect of the video modeling intervention on preoperative anxiety and postoperative behavior changes in children undergoing ambulatory surgery was assessed. The impact of the video intervention on parent anxiety was also examined. In this IRB-approved, double-blinded, randomized controlled trial, patient-parent dyads were randomized into one of two groups: the experimental group who watched the surgery preparation video and a control group who did not watch the video. Patients in both groups received child life specialist services in accordance with standard practice at the facility.
Participants
The sample size of this pilot study was based on precedent according to a meta-analysis of similar studies examining the effects of preparation and behavioral interventions on preoperative anxiety in children (Chow et al., 2016). Approval was obtained to enroll 80 patients to allow for a drop-out rate of up to 25%. Sixty patients ages 5 to 10 years old enrolled in this study between November 2020 and July 2022. Inclusion criteria was children ages 5 to 10 years scheduled for same-day surgery requiring general anesthesia. Patients were excluded if they could not complete the survey or if they had already seen the video prior to another surgery. English- and Spanish-speaking dyads were included in the study, and both the video intervention and child life services were available in English and Spanish. Eligible patients were randomized into the video group (VG;n = 34) or no video group (NVG;n = 26) using two computer-generated randomization lists due to age stratification. Patients were stratified by age (5 to 7 years and 8 to 10 years) based on cognitive development theory (Piaget, 1936/1952).
Procedures
Research assistants identified eligible patients using a surgical booking program and approached their parents during the registration process at the preoperative clinic appointment. Parent-child dyads were shown a video about child life services, and the purpose of the study was explained. Once consent was signed, participating dyads were randomly assigned to the VG or NVG.
Preoperative Visit
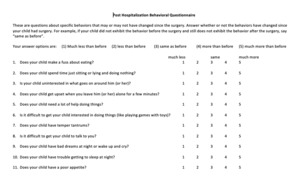
Preoperative clinic visits took place an average of 5 days prior to surgery, with a range of 2 to 42 days. Of the 60 patients, 96.7% had surgery within 15 days of their preoperative appointment. During the preoperative visit, child and parent anxiety was recorded by study staff using the Children’s Fear Scale (CFS) to establish a baseline. The CFS (Figure 2) is a one-item self-report measure of fear in children developed and tested for use in healthcare settings with children 5 to 10 years old. It is developmentally appropriate for children because it allows for nonverbal response (pointing). Psychometric testing of this tool found support for interrater reliability, test-retest reliability, and construct validity (McMurtry et al., 2011). The CFS has also been used to rate parents’ perception of children’s fear and parent-child ratings have been moderately correlated. The CFS is based off the Faces Anxiety Scale which uses the same images to measure fear or anxiety in adult patients (McMurtry et al., 2011). In this study the CFS was used to measure child anxiety (self-report) and parent anxiety (parent report). After the administration of the CFS, vital signs (e.g., respiratory rate, heart rate, and blood pressure) were recorded for each patient, as these can be an indicator of anxiety (Karakul & Bolisik, 2018; Kiani et al., 2013).
Following the recording of vital signs, families in the NVG group received standard care including a preoperative visit with their surgical team and child life specialist. In addition to standard care, the VG group viewed a video designed by a child life specialist in which a child actor depicts the perioperative sequence of events. The intervention video depicts a 10-year-old female actor and her mother, doctors, nurses, and a child life specialist. The video demonstrates a patient’s process on the day of surgery at the ambulatory surgical center.
Day of Surgery
On the day of surgery, patient and parent anxiety was recorded using the CFS before vital signs were taken. The child life specialist provided patients in both the VG and NVG groups with standard child life services offered to all surgery patients at the ambulatory center. Child life services provided to all patients included the following interventions: developmentally appropriate play activities, verbal and visual explanation of the surgery process with pictures, familiarization with an anesthesia mask, the opportunity to choose a mask flavor, and accompaniment into the operating room during anesthesia induction.
Follow-up Phone Call
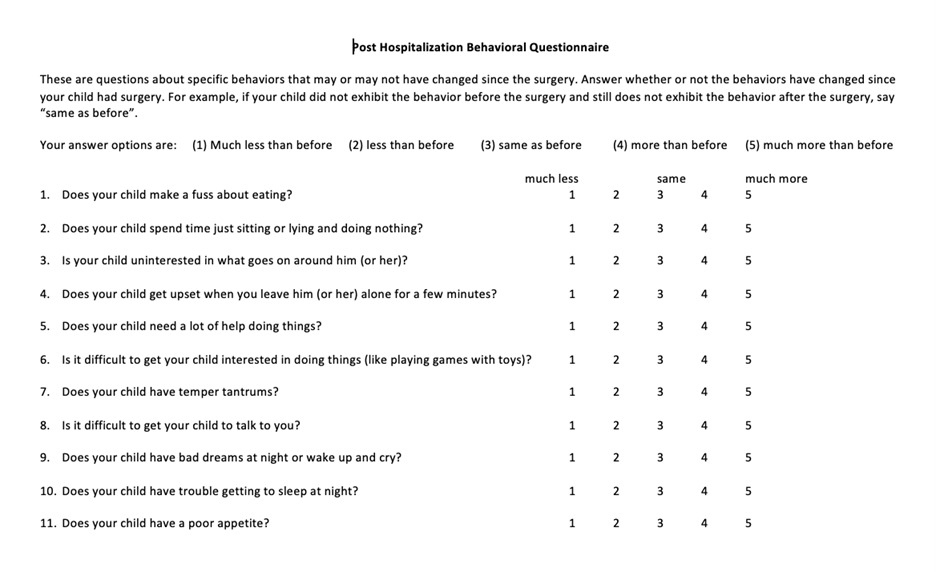
The Post-Hospitalization Behavior Questionnaire-Ambulatory Surgery (PHBQ-AS) was administered via telephone on postoperative days 2 and 14 by study staff. The PHBQ-AS (Figure 3) is a revised version of the Post-Hospitalization Behavior Questionnaire which was designed for assessing postoperative and posthospitalization new onset behavioral changes in children. The PHBQ is considered “the criterion standard” for assessing postoperative behaviors in children ages one month to 16 years old (Jenkins et al., 2015, p. 739). The PHBQ-AS is appropriate for patients undergoing ambulatory surgery. It has fared well in tests of its validity, reliability, and consistency (Jenkins et al., 2015).
Analysis
Descriptive statistics are reported as means (M) and standard deviations (SD) for continuous variables and frequencies and percentages for categorical variables. Given the non-normal nature of many of the measures and the small sample sizes, non-parametric tests were used for all comparisons of means. Specifically, comparisons of mean differences across groups used Mann-Whitney U tests, and comparisons within groups used Wilcoxon signed rank tests. Correlations were analyzed using Spearman correlations. Comparisons of proportions were conducted using Chi-Square or Fisher’s Exact tests, as appropriate. Analyses were conducted in the full sample and then stratified by patient age categories used in the randomization scheme. All analyses were conducted in SAS version 9.4 (SAS Institute, Cary, NC), and α = 0.05 was used to determine statistical significance.
Results
Sixty parent-child dyads enrolled in this study. The average patient age was 7.9 years (SD: 1.7 years), and 33 (55.0%) patients were male. Most participants reported Hispanic-Latino ethnicity (71.7%). Over half were Spanish speakers (56.7%). The majority had a prior history of surgery (61.7%). There were no statistically significant demographic differences between the intervention and control groups. Demographic characteristics by intervention group are shown in Table 1. Primary outcomes are reported first followed by secondary outcomes.
Primary Outcomes
Children’s Faces Scale – Patients
No differences in average CFS scores at the consent visit were found between children in the intervention group versus the control group (Table 2). On surgery day, CFS scores among children were significantly lower in the intervention group (M = 0.97, SD = 1.09) compared to the control group (M = 1.83, SD = 1.52; p = 0.03, r = .289), indicating that the video had a beneficial impact on children’s anxiety. CFS scores did not significantly increase from the consent visit to surgery day in either group, and the magnitude of increase across the two time points was not significantly different between groups. Results were similar when stratifying by patient age (Table 4).
Children with previous surgeries had significantly lower CFS scores at the consent visit (M = 0.58, SD = 1.05) compared to children who had no previous surgeries (M = 1.83, SD = 1.59; p = 0.001, r = .423). However, children with previous surgeries did have an increase in CFS scores between the consent visit and surgery day (M = 0.58, SD = 1.4), and this increase was significantly different from the minimal change observed among children with no previous surgeries (M = -0.17, SD = 0.91; p = 0.01, r = -.327). When the groups were disaggregated by age, the increase in CFS scores for those with previous surgeries was significantly different from the change among those with no previous surgeries among 5 to 7-year-olds only (p = 0.05, r = -.394; Table 3).
Children’s Vital Signs
No differences in vital signs between the two groups were observed at either time point (Table 4). These results persisted even when stratifying by patient age. Vital signs did not significantly change between the two time points, except the systolic blood pressure among children in the control group, which did significantly increase (M = 5.19, SD = 8.64; p = 0.02, r = .482). There were no differences in the magnitude of change between the two groups, in the full sample or when stratifying by age. Diastolic blood pressure among 5 to 7-year-olds in both groups increased across the two visits (M = 8.42, SD = 7.48 for intervention; M = 8.33, SD = 10.27 for control), though the increase was only significant in the intervention group (p = 0.01, r = .679).
Among 5 to 7-year-olds, in the intervention group, there was a marked reduction in heart rate between the two visits, though this was not statistically significant (M = -5.85, SD = 12.47; p = 0.07). In 8 to 10-year-olds, children in the intervention condition had a significantly lower respiratory rate on the day of surgery compared to those in the control group (M = -2.72, SD = 4.00; p = 0.01, r = .006).
Children’s Faces Scale – Parents
There was no significant difference in the average CFS score for parents at the consent visit in the intervention group compared to the control group (Table 2). Similarly, no differences in the average CFS score between the intervention or control groups were observed on surgery day. Increases in parent CFS scores from the consent visit to surgery day were not significant in either the intervention or control group, and the magnitude of the increase was also not significantly different. These conclusions remained the same after stratifying by the age of the parent’s child.
Parents whose children had a previous surgery reported lower CFS scores at the consent visit (M = 0.95, SD = 1.2, Table 3) than parents whose children did not have a previous surgery (M = 1.7, SD = 1.11; p = 0.01, r = .331), consistent with the children’s CFS scores. This finding was attenuated in parents of 5 to 7-year-old children. However, among parents of 8 to 10-year-old children, this finding still held (M = 0.50, SD = 0.73 for parents of children with prior surgery; M = 1.83, SD = 1.04 for parents of children with no prior surgery; p < 0.001, r = -.594). Parents of 8 to 10-year-old children with prior surgery had a significantly greater increase in CFS scores from the consent visit to surgery day (M = 0.75, SD: 1.00) than parents of children with no prior surgery (M = -0.06, SD = 1.06; p = 0.033, r = -.378).
Post Hospitalization Behavior Questionnaire – Ambulatory Surgery
The average PHBQ-AS score for children two-days post-surgery did not differ between the intervention or control group (Table 5). This finding persisted at 14 days post-surgery. When stratifying by the child’s age, no differences in the mean scores across intervention and control group were observed at either time point.
However, the intervention group showed significant reductions in PHBQ-AS scores over time (M = -1.33, SD = 2.71, p = 0.002), although the magnitude of the reduction was not meaningfully different between the two groups (p = 0.25). For younger children, the reduction of PHBQ scores was not significant in either group; whereas, for older children the reduction of PHBQ scores in the intervention group was significant (M = -1.59, SD: 2.53, p = 0.01, r = .241), indicating that the video intervention had a beneficial impact on post-hospital behavior changes for 8 to 10-year-olds. Conclusions regarding the magnitude of differences also remained the same when stratifying by child’s age.
When comparing PHBQ-AS scores among children in the full sample who had previous surgeries to those who did not, no meaningful differences were observed at two days post-surgery, 14 days post-surgery, or in the magnitude of change across the time points. However, when stratifying by age, children 5 to 7 years old who had previous surgeries had significantly lower PHBQ scores at two days post-surgery (M = 34.00, SD = 1.76; Table 3) than those who had no previous surgery (M = 36.6, SD = 2.88; p = 0.039, r = .404), but no such differences were observed among children 8 to 10 years old. Additionally, when considering the intervention groups, first-time surgery patients in the control group had higher post-hospital behavior scores two weeks after surgery (M = 34.13, SD = 1.73) than their peers who had undergone surgery before (M = 33, SD = 1.46; p = .04, r = .37), indicating that the video intervention may have contributed to reduced post-hospital behaviors for first-time surgery patients.
Secondary Outcomes
Comparing Patient-reported Measures across Sex and Language
Females in the control group had significantly higher PHBQ scores at two days post-surgery than males (M = 35.90, SD = 3.81 and M = 33.25, SD = 1.06, respectively; p = 0.012, r = .450) and had a greater reduction in PHBQ scores across the two time points (M = -2.80, SD = 2.70 and M = 0.25, SD = 1.29, respectively; p = 0.003, r = -.529; Table 6).
At the consent visit, English-speaking children in the intervention condition had significantly higher CFS scores than Spanish-speaking children (M = 1.41, SD = 1.46 and M = 0.13, SD = 0.34, respectively; p = 0.002, r = -.565; Table 7). On surgery day, English-speaking children in the control condition had significantly higher CFS scores than Spanish-speaking children (M = 2.81, SD = 1.07 and M = 1.39, SD = 1.5, respectively; p = 0.029, r = .392), but no differences were observed between English and Spanish-speaking children in the intervention group.
Correlations
Child CFS scores were significantly correlated with parent CFS scores at both the consent visit (Spearman correlation [ρs] = 0.326, p = 0.012; Table 8) and on surgery day (ρs = 0.445, p < 0.001). The relationships persisted in the sample of children 8 to 10 years old (ρs = 0.694, p < 0.001 at consent visit; ρs = 0.509, p = 0.003 on surgery day; Table 10). Among children 5 to 7 years old, child CFS scores were significantly correlated with parent CFS scores on surgery day (ρs = 0.397, p = 0.044), but not at the consent visit (p = 0.56; Table 9). No significant correlations between child or parent CFS scores and PHBQ-AS scores were observed at either time point.
Discussion
This study was conducted to add to the literature on child life specialist services and the impact of preparation interventions on pediatric surgery patients and their parents. The study results confirm the findings of previous studies that video modeling can reduce children’s preoperative anxiety and regressive post-hospital behaviors. When added to standard child life preparation interventions, video modeling, in which a child (patient or actor) proceeds through the impending healthcare process, provides significant benefit to children ages 5 to 10 years undergoing outpatient surgery. In this section, primary outcomes of the analysis are discussed, followed by a review of the impact of several confounding variables.
Primary Outcomes
Child and Parent Preoperative Anxiety
While CFS scores in both the intervention and control groups increased as expected from the consent visit baseline to the day of surgery, children who received the video modeling intervention exhibited significantly lower anxiety than children in the control group. This finding indicates that the video modeling intervention had a significant positive impact on children’s preoperative anxiety beyond the impact of standard child life services received by all children in both groups.
Research has found that parental anxiety has a significant negative impact on children’s preoperative anxiety (Getahun et al., 2020; Liu et al., 2022). The study findings confirm a relationship between the two, finding that child and parent anxiety were significantly correlated across age groups on the day of surgery. However, no statistical difference was seen in parental anxiety between the control and intervention groups. Several possible explanations exist. Parents receive information about the surgery process from medical providers. Perhaps the video, which was designed to communicate to children about surgery in a developmentally appropriate way, did not provide any substantially different information beyond what parents already knew. Additionally, sources of parental anxiety and child anxiety regarding a child’s surgery may differ. For example, as an intervention directed at children, the video does not address risks of surgery or detailed information about recovery, nor is it specific to the type of surgery each patient may be having. Finally, despite the evidence of the appropriateness of faces scales for measuring adult anxiety (Gustad et al., 2005; McKinley et al., 2003, 2004) and the use of the CFS in a previous study for parent perception of child anxiety (McMurtry et al., 2011), there may be a more sensitive instrument available for measuring anxiety in parents of children undergoing surgery.
As an additional indicator of child anxiety, we examined children’s vitals (e.g., blood pressure, respiratory rate, and heart rate). While no significant differences in vital signs were seen between groups at either time point, significant differences in changes over time were observed between groups. Although most physiological results were non-significant, children in the control group experienced a significant increase in systolic blood pressure between time points 1 and 2 which children in the intervention group did not experience, offering further support for the beneficial impact of the video preparation on anxiety. Finally, among children 8 to 10 years old in the intervention group, respiratory rate decreased between time points 1 and 2, indicating that the video preparation may have contributed to reduced anxiety for this age group.
Children’s Postoperative Behavior Changes
Children in the intervention group experienced a significant decrease in regressive post-hospital behaviors (PHBQ-AS scores) between days 2 and 14 post-surgery, indicating that the video modeling intervention had a positive impact on post-surgery behavior changes. After disaggregating the intervention group by age, the decrease over time remained significant for older (8 to 10 years) children in the intervention group but not for younger (5 to 7 years) children. These results may indicate that the video intervention was most effective at reducing distress leading to post-hospital behavior changes for children 8 to 10 years old. Of note, the video intervention included reassurance about the possibility of waking up with discomfort following surgery as well as suggestions for coping with that discomfort. It is possible that the inclusion of this information was of more benefit to older children who have a greater cognitive capacity than younger children to consider future possibilities.
Secondary Outcomes
The interactions of preoperative anxiety and post-hospital behaviors with several variables indicated in the literature were examined to determine whether they played a significant role in pediatric patients’ outcomes. The impact of age, gender, language, and previous surgery history was explored.
Between-group Differences in Preoperative Anxiety
The research on the relationship of age to preoperative anxiety is conflicting. In this study, patients in the intervention group displayed significantly lower anxiety on the day of surgery than those in the control group. However, when examining the disaggregated age groups, the differences in CFS scores were no longer significant, likely due to the small size of each group. Although not statistically significant, among the 8 to 10-year-olds, the increase in anxiety over time was smaller for the children who saw the video than for those who did not. Meanwhile, the change over time was the same for the 5 to 7-year-olds in both groups, indicating the preparation intervention may have had a larger impact on anxiety for the older patients. These results should be interpreted with caution due to the small sample size.
A history of previous surgery is a risk factor for increased preoperative anxiety in children (Getahun et al., 2020). In this study, children 8 to 10 years old who had experienced a prior surgery and their parents had significantly lower anxiety at the consent visit compared to first-time surgery patients and their parents; however, similar anxiety scores on the day of surgery were seen in both groups. In contrast, children 5 to 7 years old who had a previous surgery exhibited similar levels of anxiety to their first-time peers at both time points, but their anxiety increased over time, while the anxiety of children with no prior surgery decreased over time. These findings underscore the importance of perioperative support for children who have already undergone a surgery, while emphasizing that preparation prior to the day of surgery is of paramount importance for first-time surgery patients.
Between-group Differences in Post-hospital Behavior Changes
In contrast to the findings of Quiles and colleagues (2000), no gender differences were observed in preoperative anxiety scores in our study; however, female children in the control group exhibited significantly more post-hospital behaviors than males two days post-surgery. In contrast, no significant difference was seen between genders in the intervention group, indicating that the preparation intervention may have mitigated the impact of gender on post-hospital behaviors.
Although Fortier and colleagues (2012) found that cultural variables influence parent report of post-hospital behavior changes in children, this study found no significant differences in PHBQ-AS scores at either time point between English- and Spanish-speaking patients. Of note, Fortier and colleagues used the full 27-item PHBQ and enrolled a larger patient sample than our study. It may be that this study’s sample size was not sufficient to detect between-group differences once disaggregated by language group.
In this study, a history of prior surgery was correlated with fewer post-discharge behavior changes. Children ages 5 to 7 years old who had previous surgeries had significantly lower PHBQ-AS scores at two days post-surgery than their peers who had no previous surgery. However, this difference disappeared by the fourteenth day. However, in the combined sample (ages 5 to 10), first-time surgery patients exhibited more post-hospital behavior changes two weeks after surgery than their peers, but only among the control group. These results suggest that first-time pediatric surgery patients are more at risk for regressive post-hospital behaviors than children with a history of surgery. In addition, the higher scores among first-time surgery patients in the control group compared to their peers in the intervention group indicates the video intervention may have contributed to reduced post-hospital behaviors for first-time surgery patients.
Limitations
Some limitations were present in this study, including a small sample size. Although this pilot study mirrored the sample sizes of several similar studies (Batuman et al., 2016; Fincher et al., 2011; Kain et al., 2001), the sample size may have limited the ability to detect between-group differences in the stratified groups. The COVID-19 pandemic impacted the study team’s ability to collect additional data due to reduced scheduling of elective surgeries and postponements for international patients. An IRB extension was requested, and data collection was extended an additional year to allow the minimum desired sample size of 60 patients to be reached. Due to the unanticipated need to significantly extend our data collection period, the study team concluded collection prior to reaching the preferred goal of 80 participating dyads.
Additionally, the Spanish versions of the CFS and PHBQ-AS used in this study have not yet been validated. A recommendation for future research is to conduct a full validation study of the Spanish language instruments. Finally, the CFS scores were nonnormally distributed, likely due to the small range of score options (0 to 4). However, statistical tests were used to account for this feature of the collected data. Additionally, the distribution reflected the distribution of fear ratings seen in a study of the psychometric properties of the instrument by McMurtry et al. (2011) in which scores were significantly positively skewed.
Recommendations and Implications
This study confirmed findings from previous studies that video modeling, when provided prior to the day of surgery, is an effective intervention for reducing pediatric preoperative anxiety and postoperative behavior changes. Video modeling can be incorporated into the preparation interventions provided by child life specialists. Given the known relationship between parent and child anxiety, interventions to reduce parental preoperative anxiety could benefit pediatric patients as well. Additionally, this research can lend weight to advocacy for implementation of child life services in perioperative settings and for resources to create evidence-based video modeling tools.
Future research could assess the impact of video modeling on younger (<5 years) and older (>10 years) surgery patients as well as the impact on children undergoing non-surgery procedures or other stressful healthcare encounters. Additionally, future studies could compare the impact of receiving a video preparation to other types of preparation techniques. Finally, this study did not control for the length of time that passed between patients’ viewing of the video and their surgery; future research could explore the optimal timing of a video preparation intervention.
Conclusion
This study found that an informational video designed by a child life specialist is an effective tool for reducing preoperative anxiety and postoperative behavior changes in children ages five to ten years old undergoing ambulatory surgery. The video intervention benefitted patients when added to the provision of standard child life specialist services. Video modeling interventions, particularly when informed by the expertise of a child life specialist, are a useful modality for preoperative preparation of pediatric patients.