Introduction
A Certified Child Life Specialist (CCLS) is a skilled, typically pediatric-facing member of the healthcare team that prioritize the developmental and psychosocial wellbeing of children and their families (Boles et al., 2020). More specifically, CCLSs accomplish these aims by providing psychological preparation and individualized comfort interventions during painful or distressing medical procedures (Romito et al., 2021). These therapeutic interventions are adapted for each individual patient and all pediatric specialties. Furthermore, these interventions are documented by an impressive catalogue of research demonstrating the individual and institutional benefits of child life services for patients and communities (Boles et al., 2020; Pillai, 2020; Romito et al., 2021).
Children’s health care experiences and procedural pain, specifically surgery, have been well studied, attesting to the recurrence and continuation of healthcare-related anxiety into adulthood if not addressed at the time of onset (Cohen, 2008). Additional evidence demonstrates the added benefit of these essential allied health care professionals as they teach pediatric patients age-appropriate coping skills that will reduce pain, anxiety, and distress in a variety of health care encounters and settings (Boles, 2016; Boles et al., 2020; Romito et al., 2021). The American Academy of Pediatrics Child Life Services Policy Statement (2021) affirms, “Child life services are part of an integrated patient and family-centered model of care and can be used as a quality measure in the delivery of health care services for children and families” (p.7).
Although child life services are multifaceted, the effects of child life interventions, specifically on children’s pain perceptions and experiences, are particularly noticeable. Not only are child life interventions like preparation and procedural support associated with decreased pain ratings, but they are also associated with decreased need for pain management medications and less use of sedation during stressful procedures. Much of this evidence is specifically garnered from pre-operative and surgical settings where children are experiencing highly invasive procedures with a similarly high likelihood of pain. Furthermore, parents/guardians of patients receiving child life services in these settings report greater satisfaction with their child’s care in these encounters and at times report decreased stress for themselves (Boles et al., 2020).
Such findings necessitate a continued line of inquiry and practice improvement: if child life services have been implemented with such success in improving psychosocial outcomes for children, why have similar opportunities not yet been afforded to the adult population (whom children one day will become) to support the development and use of effective coping skills that will enhance healthcare experiences throughout the lifespan? As posed by Jason Wolf, CEO of the Beryl Institute (2018), “why are we not providing the same level of professional service beyond the pediatric settings?” (p. 3). Adult health care does not currently offer the robust psychosocial support that is standard of care in the pediatric healthcare world. Child life’s fundamental framework encapsulates care for patients and families in the broadest sense. In adult settings, social work, psychology, spiritual care, and other allied health professions typically have higher patient to clinician ratios than in pediatrics and are often consult based. With the disparate gap in supportive care services for adult health care, expanding any of these services would be valuable for adult patients and their families. Child life specialists have an opportunity to fill this void through their unique qualifications and skill set.
Literature Review
Due to their age, most health care providers consider adults to have more life experiences and subsequently more knowledge about implementing coping strategies in their health care encounters. Contradictory to this assumption, anticipatory anxiety related to procedures, including cardiac surgery, has been well documented in adult patients (Ai et al., 2007; Leach et al., 2000; Pignay-Demaria et al., 2003; Voss et al., 2004). Adults report pain and fears, and they can also build longer associations with unmitigated anxiety (Cohen, 2008; Horovitz et al., 2012). Furthermore, false assumptions can contribute to clinician-related barriers to care including displayed personal and cultural implicit and explicit bias towards the adult patient, pain management knowledge deficits, and failure to assess and acknowledge pain existence (Pasero, 2009). Evidence indicates lingering long-term negative effects from earlier painful encounters can have lasting detrimental effects on neuronal development, pain threshold and sensitivity, coping strategies, emotionality, and pain perceptions (Cohen, 2008; Horovitz et al., 2012; Porter et al., 1999; Taddio et al., 1999). Likewise, childhood medical-related pain has also been associated with later adulthood pain, fear, and avoidance of medical care (Pate et al., 1996). Therefore, a considerable number of adult patients struggle with anxiety and bring their struggles into their adult health care experience without having support to develop effective coping strategies for their current surgical experience.
This anxiety concept has been especially noted in patients having cardiac surgery (Kok et al., 2016). In a study by Tully and colleagues (2011), it was further noted that anxiety symptoms in the postoperative period were associated with atrial fibrillation (AF). Tully and colleagues (2011) indicated the need for hospital staff in acute cardiac care and cardiac rehabilitation settings to observe anxiety as related to AF after cardiac surgery. While not clear how anxious cognitions influence the experience of AF symptoms, their findings support further study on the implications of anxiety in AF and recommend that hospital staff in acute cardiac care and cardiac rehabilitation settings be aware of anxiety’s potential effects on patient outcomes. (Tully et al., 2011).
Perioperative anxiety in adult surgical patients has been well-documented and is widely understood (Calvin & Lane, 1999; Goodwin et al., 1999; Hölzel et al., 2010; Hyman et al., 1989; Kabat-Zinn & Hanh, 2009; Leach et al., 2000; Pasero et al., 1999; Voss, 2001; Voss et al., 2004; Wiens, 1998; Williams, 2006). Apart from producing emotional upset ranging from discomfort to debilitating panic and avoidance, anxiety may also adversely affect patient outcomes including in-hospital recovery and understanding of post-discharge care (Centers for Disease Control and Prevention, 2013; Kulik et al., 1996; Orr, 1986; Shuldham, 1999). Not only is anxiety a factor in patient outcomes but pain has also been noted to cause stress, which in turn causes the cardiovascular system to activate the sympathetic nervous system. This activation results in increased heart rate, blood pressure, and oxygen demand- all which can have a negative impact on recovery after open heart cardiac surgery (Dezfouli & Khosravi, 2020; Tully & Baker, 2012). These effects have generated a longstanding empirical interest in psychosocial factors present when patients undergo open heart cardiac surgery that may increase risk of morbidity in the short and longer term. Evidence supports findings that both depression and anxiety increase the risk for mortality and morbidity after cardiac surgery independent of medical factors (Tully & Baker, 2012). Non-pharmacologic interventions are recognized as simple, valuable, and inexpensive tools as an alternative or complement to pharmacologic treatment for pain management (Dezfouli & Khosravi, 2020; Hyman et al., 1989; McCaffery, 1990; McCaffery & Robinson, 2002; Skelly et al., 2018; Tick et al., 2018).
Within pediatric healthcare, CCLS are primary providers facilitating evidence-based, effective non-pharmacologic pain and anxiety management interventions to support patient understanding, coping, and comfort when preparing for and experiencing painful procedures (Bandstra et al., 2008; Boles et al., 2020; Gursky et al., 2010; Tick et al., 2018; Zempsky et al., 2004). This type of support and its targeted efforts to reduce stress and anxiety by facilitating non-pharmacologic pain management is currently missing in the adult patient experience. At this juncture, there appears to be more evidence for implementing non-pharmacologic interventions in pediatric patients undergoing painful or invasive procedures than in the adult care setting–perhaps due to the prevalence of child life presence (Bandstra et al., 2008; Gursky et al., 2010; O’Brien et al., 2015). One well documented pediatric intervention in this vein is psychological or stress-point preparation, which increases understanding while decreasing misconceptions, fear, anxiety, and pain, while providing a context for the specialist’s assessment of immediate and longer-term coping needs to inform plans of care (Fincher et al., 2012; Sanchez Cristal et al., 2018).
Non-pharmacologic interventions are increasingly employed in adult health care settings to prevent and mitigate stress, anxiety, and pain. In adult populations, these efforts have been shown to decrease adverse mental and physical health outcomes (Kolcaba et al., 2006; McCaffery, 1990). Specifically in adult cardiac surgery patients, this inclusion of a non-pharmacologic pain control dimension can also enhance the patient’s individual strengths and resilience in coping with future clinical interventions and experiences (Ai et al., 2007). Additional evidence supports specific non-pharmacologic interventions such as music and relaxation that help reduce pain post-operatively in adult patients having open heart surgery (Özer et al., 2013).
When nonpharmacological techniques are offered in conjunction with effective pharmacological methods of pain control, the most successful pain relief and coping support for the patient is achieved (McCaffery, 1990; U.S. Department of Health and Human Services, 2019). Despite this evidence, there are no staffing resources comparable to child life services offered for most adult patient populations undergoing stressful and painful procedures such as surgery or hospitalization. Therefore, the purpose of this pilot study was to explore 1) the practical feasibility of extending and integrating child life care into the adult cardiac surgery service as well as 2) the preliminary perceptions of staff and patient stakeholders who participated in the pilot program.
Cardiac Adult Care
Cardiac surgery is well documented as an extremely traumatic experience from a physical, emotional, and psychological perspective causing high levels of pain and anxiety in both patients and families, often resulting in an overall poor medical experience (Bjørnnes et al., 2016; Goodwin et al., 1999; Hernández-Palazón et al., 2018; Koivula et al., 2001; Pagé et al., 2017; Voss et al., 2004). Historically, narcotic pain medications have been used as frontline therapy to help manage patient pain after cardiac surgery, with hardly any attention to psychological pain confounds such as anxiety and fear (Brescia et al., 2019, 2021). With the recent recognition of the opioid crisis in the United States in the 21st century, hospitals have shifted their attention away from these documented pharmacological pain management strategies and instead generated protocols that minimize post-operative narcotic distribution. Although this may prevent long term opioid-related use and misuse, such policies also change the landscape of pain management for patients and families and can thereby heighten anxiety in all categories of post-operative surgical patient populations (Brescia et al., 2021; Clement et al, Wagner et al., 2021).
Recipients of cardiac surgery have been shown to be one of the top surgical specialties primarily caring for patients who identify as opioid-naïve; at the same time, cardiac surgery also produces a high proportion of chronic post-operative opioid users (Dewan et al., 2019). Therefore, intentional research efforts have turned to decreasing opioid distribution and dependency for this specific patient population (Allred et al., 2010; Dewan et al., 2019; Hill et al., 2017; Howard et al., 2019), employing music engagement, relaxation, guided imagery, visual arts, and quiet rest periods to decrease pain and anxiety over time. Considering the also well-documented pain-related benefits of child life services and current widespread efforts to reduce overuse of opioid pain medications in adult patients having cardiac surgery, a collaborative pilot program was created to explore the possibility of child life services in pre- and post-operative care for this population.
Current Study
Rather than diving into a randomized controlled clinical trial, the team identified a host of unanswered logistic questions that would need to be initially addressed. First, would adult patients and their families be receptive to a CCLS delivering non-pharmacologic interventions in place of unrestricted narcotics? Second, would it be feasible to integrate a seasoned CCLS used to working in pediatric health care into the adult cardiac surgery care team (ACSCT) as an accepted, respected, and valued contributing team member? Third, with regard for patient experience, what tools would adult patients prefer to try and find useful for non-pharmacologic pain management, and when and how would they prefer to access these strategies?
With these needs in mind, this pilot study was undertaken to gather information that would create a foundation for future systematic study and program development. Therefore, bringing together the imminent need for non-pharmacologic solutions for pain and anxiety within the adult cardiac surgery patient population and the long-documented history of child life service efficacy within the pediatric patient population, the Department of Cardiac Surgery and the Office of Patient Experience partnered with the Department of Child & Family Life to pilot a child life-led pain management program in the adult cardiac surgery patient population. The two central aims of this pilot program were to explore:
-
the practical feasibility of extending and integrating child life care into this adult healthcare service, and
-
the preliminary perceptions of adult participants and staff stakeholders involved in this pilot program.
By achieving these aims, future programs can consider the costs and benefits of extending child life services into other adult health care settings and populations as a means for promoting non-pharmacological pain management techniques post-surgery and aiding in the adjustment to healthcare experiences.
Method
This pilot program was implemented and evaluated at an academic medical center in the midwestern United States. The facility is adjacent to a children’s hospital with a robust child life department that is available on a consult basis 24/7 for the children of adult patients. The child life department at this site has seen increased referrals over the past several years for adults in settings such as radiation oncology (which has shared pediatric and adult waiting spaces), procedural support for developmentally delayed patients with high anxiety, and increased referrals related to needle phobia and procedural distraction support for typically developing adults. An individualized procedural pain plan was developed in pediatric settings at the site and has been adapted and implemented for adult patients in recent years. This system-wide intervention has increased awareness of the benefits of coordinated non-pharmacologic pain management strategies and individualized coping support across nursing, social work, the medical pain management service, and child life. For this pilot program, cardiac surgery was chosen because of the high risk of trauma associated with open heart surgery and the medical department’s interest in better managing opioid pain medication use in this population.
During the first phase, the initial concept for this study was presented to an advisory panel of former patients and families to obtain their feedback about the need for, design of, and essential considerations for application of child life support to adult patients undergoing cardiac surgery. Crucial information was gathered about proposed timing of recruitment, the spectrum of coping interventions offered, and ways to successfully integrate care into the flow and processes of the adult cardiac surgery team. Concurrently, the initiative was proposed to the child life team of the affiliated children’s hospital to assess which specialists may be interested in and have the capacity to participate as the interventionists in this developing pilot program. The resulting intervention team was jointly selected by the leaders of the Office of Patient Experience and Department of Child & Family Life, with specific attention to experience with adult care referrals, non-pharmacologic interventions, procedural preparation, confidence with interdisciplinary team collaboration, and willingness to try something new. Once the team was solidified, feedback from the key stakeholder panels was integrated into the formal pilot program protocol and institutional review board submission documents.
Participants
The participants in this pilot program included 11 adult patients scheduled to undergo cardiac surgery who were at least 18 years old at the time of participation and were receiving their first open heart cardiac surgery (see Table 1). All participants were between the ages of 40 and 80, and the sample was primarily White (80%) patients who identified as male (80%). Excluded from participation were those who were non-English speaking, had undergone previous heart surgeries, demonstrated an inability to understand or complete surveys without assistance, those who self- or caregiver-reported significant medical or psychiatric conditions that would preclude participation in the study, individuals who were pregnant, and those unable to independently sign a legal consent form on their own behalf. This study was approved by the Institutional Review Board (IRB) and was designed in compliance with the Helsinki recommendations for ethical scientific study with human subjects.
Procedures
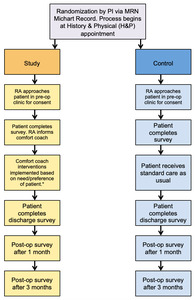
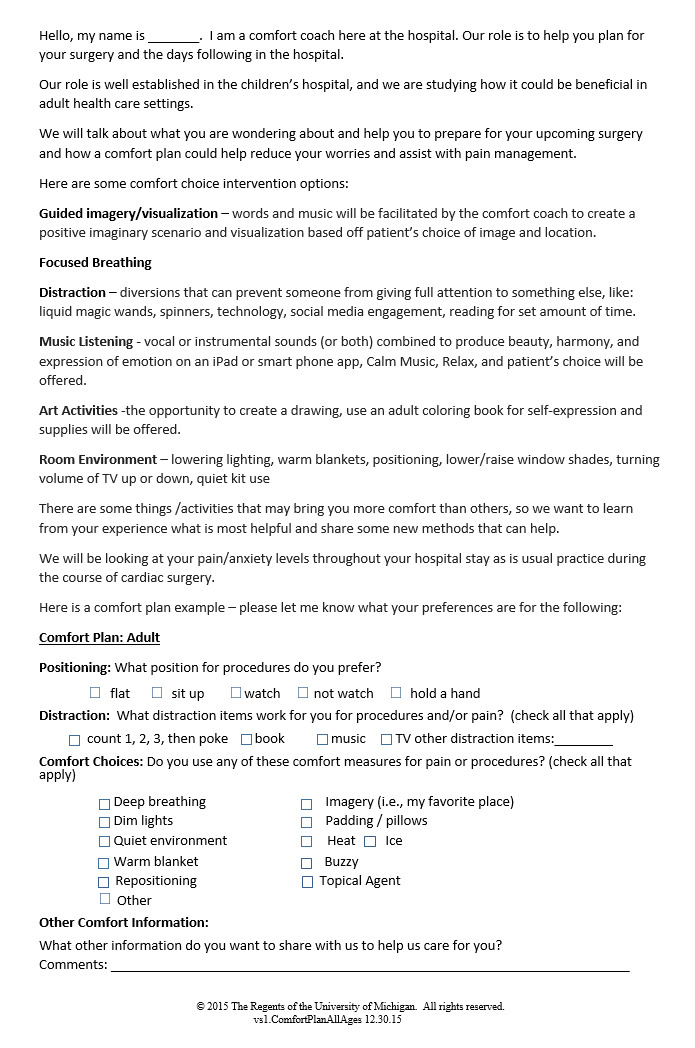
The overarching pilot study protocol was constructed as a randomized, prospective double arm feasibility study comparing a control group receiving standard cardiac surgical care and an experimental group receiving individualized non-pharmacologic child life coping interventions in addition to standard care (see Figure 1). The intervention group participated in five interactions with a CCLS that aligned with what the patient and family panel identified as the most important timepoints in the cardiac surgery timeline: 1) the pre-operative out-patient clinic visit, 2) post-anesthesia care unit prior to surgery, 3) intensive care unit stay, 4) just prior to discharge on the stepdown unit, and 5) at discharge on the stepdown unit.
Trained research assistants screened medical charts to identify patients who met the study inclusion criteria. Eligible patients were approached by a member of the study team in the preoperative clinic waiting area at their initial History and Physical (H&P) appointment prior to being scheduled for surgery. Research staff introduced the purpose of the research study, the randomization process, and the potential risks and benefits of the study. After signing the consent form to participate in the study, participants were randomly assigned to the experimental study (n=5) control (n = 6) arms.
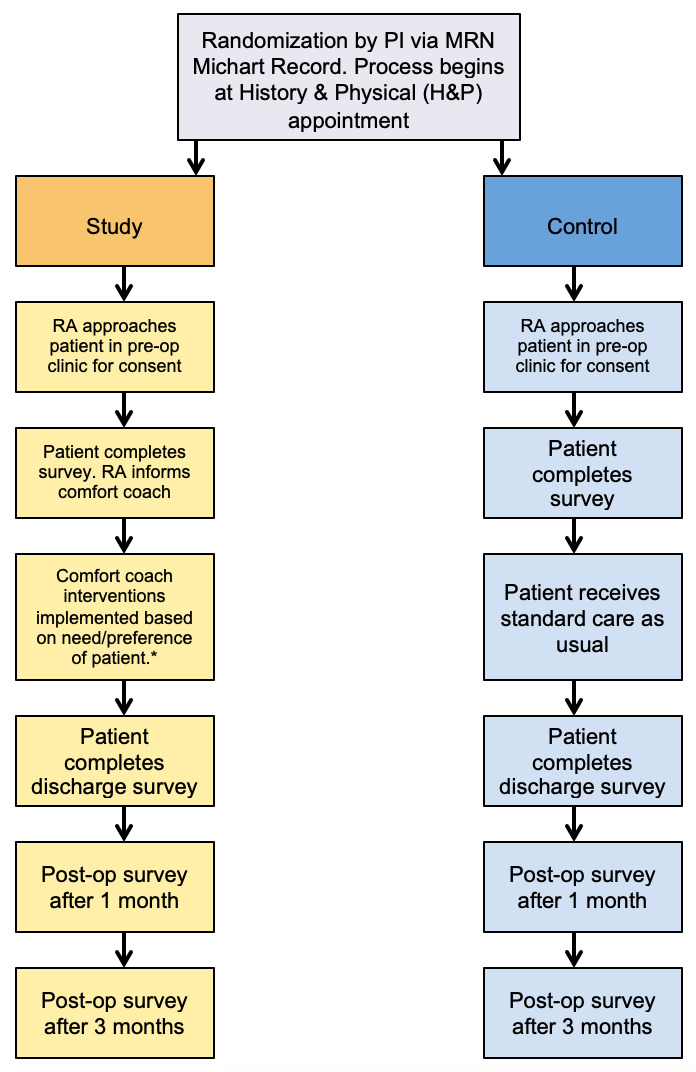
Those assigned to the experimental group were first introduced to the role of the child life specialist with the oral script utilized by the CCLS-RT in Figure 2. These patients then completed a brief survey after consenting to participate, as well as an introductory needs assessment with a CCLS during their H&P exam clinic visit. This needs assessment was used to consider the potential impact of the participant’s identified emotional, medical, and social stressors, as well as their perceived level of family support. during this same clinic visit, preparation for surgery and postoperative hospitalization was provided by the CCLS. Then, starting with the day of surgery, four additional CCLS visits were provided, with a goal of helping participants choose and use individualized comfort interventions such as guided imagery/visualization, breathing exercises, distraction, music listening, art activities, and environmental modification. Finally, follow-up surveys were administered at discharge and at 30 and 90 days postoperatively via phone or a short in-person meeting per patient preference.
Patients assigned to the control group received standard surgical care without child life preparation or focused coping support interventions. After consenting to participate, the control group completed the same entry survey as the experimental group. Then, after discharge, they were contacted by phone or email (per the participant’s preference) to complete the same series of follow up surveys.
At the conclusion of the feasibility study, the research coordinator facilitated oral qualitative interviews with the four CCLS team members and ACSCT members. The Patient-Family-Staff Advisory Council members also participated in oral semi-structured interviews with the research staff after the conclusion of the feasibility study. This group included former cardiac surgery patients, families, and interdisciplinary team members who had interfaced with the CCLS role.
Additional phone surveys were administered by a research assistant (graduate social work intern) after the feasibility study completion with both control and experimental study patients to learn more about their patient experience and to develop plans for a future larger randomized prospective clinical trial. The additional phone surveys took an average of 10 minutes to complete. All 11 participants were called and asked a series of follow-up questions, respective to their experimental or control assignment (see Tables 2 and 3).
Both the experimental and control groups completed the section about their overall patient experience, with some additional questions focused on whether they did or did not receive the study intervention. Questions for the intervention group were directed at intervention timing, perceived benefit, and acceptability whereas the control group was asked to comment on their perceptions of what it would be like to have a person (CCLS) in a dedicated role to support pain, anxiety, and preparation throughout their surgery experience. Of note, these same questions were used for all semi-structured interviews with the interdisciplinary cardiac surgery team related to understanding their perceptions of the value of a CCLS role with adult patients.
Analysis
The intent of this pilot program was exploratory. The research team reflected on the spectrum of their experiences designing, implementing, and conducting the pilot program with attention to the feasibility and practical considerations that came with adapting child life intervention for adult patients undergoing cardiac surgery. Given the novel integration of child life care into adult cardiac surgery care, the purpose of this pilot study was to explore the practical feasibility of extending and integrating child life care into this adult healthcare service, as well as explore the preliminary perceptions of adult participants and staff involved in the pilot program. As such, the goals of the study included observing physical logistics and gathering information from all involved on their impressions of the presence and benefit of the CCLS skills and tools for adult cardiac surgery care.
Results
Study Feedback
Scope of Practice
The CCLS-RT experience integrating into the adult cardiac surgery patient care environment was explored; it was found that scope of practice was an ongoing conversation within the research team and across participating child life specialists, multidisciplinary stakeholders, senior leaders, and the primary investigators. In determining the appropriateness of using child life specialists in this role, careful consideration was given to their specific skill sets that could be potentially transferable to serving adult populations. These included: preparation, procedural support, nonpharmacologic pain management, diagnosis education, development of coping skills, anxiety management, patient and family-centered care, individualized care plans, as well as assessment of and attention to the emotional safety of patients and families.
Data Collection Challenges
Several logistical challenges became apparent to the study team during the pilot program while other obstacles were communicated when collecting post-study feedback from staff and patient participants. These challenges included missed survey time points due to difficulty coordinating contact, misconceptions and assumptions about the intervention experience, and difficulty deploying and maintaining child life involvement and presence in a separate building across campus from their usual pediatric unit assignments. Even with careful and consistent recruitment efforts and the inclusion of part-time staff and graduate interns in data collection and analysis, it was difficult to create and maintain a dedicated recruitment schedule.
Family-centered Care
The CCLS-RT operated from the assumption that pain management interventions were more individually driven, rather than family-focused, in an adult patient population. However, findings from the participant feedback surveys highlighted how family and relatives are key coping supports in the healing and emotional well-being of even adult patients. Because the feasibility study did not include interaction with or data collection from family members, it is possible that useful information about coping mechanisms in context was lost. Interestingly, some of the intervention group participants reported ways in which their families were also benefiting from the CCLS-RT interventions; it appears then that family interaction and socialization with the CCLS could be an additional patient-preferred mode of pain management.
Research Staffing Challenges
Not having a fully dedicated research CCLS assigned to the feasibility study meant intervention and survey data collection points were occasionally missed or subject to variations based on the style of each individual specialists. The four research CCLSs maintained dual roles during the study, working full-time in the children’s hospital and simultaneously on-call as the research CCLS for the adult cardiovascular center. Given the expansive size of the research site, the CCLSs were not always able to arrive on time to perform the adult CCLS-RT interventions for patients in the experimental group. The comfort coach CCLSs specifically reflected afterwards this was often “due to competing pediatric clinical needs and travel distance to the adult care setting in the cardiovascular center.” Staff also noticed this difficulty as, “there needs to be a dedicated person to meet the study protocol effectively versus part-time on-call support from another building.” It appears that a full-time dedicated research CCLS would improve intervention fidelity and consistency of data collection points.
Support Staff Title
In a more philosophical vein, it was observed during this study that the title “child life specialist” was thought provoking. The term was found to be unclear and unfamiliar for adult providers and study participants, and “adult life specialist” was likewise ambiguous. More consideration of terminology and its translation to adult care will be necessary for future research in this area.
Program Perceptions
In terms of stakeholder perceptions of the pilot program, several insights were gained. According to interview responses gathered from child life specialist comfort coaches, medical staff, and participants in this pilot program, it appears that the program was well-received by all stakeholders. The CCLS-RT commented on the positive experiences overall that despite the challenges, “it was nice to see we were making a difference and helping support patients and families in the care journey,” and “the patients and families and staff were so appreciative of the support (our team) provided.”
Provider Perceptions of Child Life
Next, the team explored provider perceptions of child life specialist involvement and the cardiac care team’s experience and work environment. Cardiac surgery staff members reported that the child life role “is a much-needed service in cardiac care, as patients (undergoing cardiac surgery) are often frightened and have high anxiety.” The interdisciplinary staff further emphasized the necessity for such services stating, “we need to provide support for patients and families to help reduce the fears that often come up.”
Participant Perceptions of Child Life
In terms of participant perceptions, a total of three out of five intervention group participants completed the telephone post-survey, with two experimental patients who were unable to be reached after three attempts. All six control group participants completed the telephone survey. Participant responses indicated that CCLS-RT primarily helped with anxiety and stress brought on by the anticipation of pain as well as the emotional and physical discomfort. As one control group participant stated, “I felt uncomfortable in the evening after surgery…distraction/relaxation would be helpful then, or anytime someone feels uncomfortable.” According to an intervention group participant, “I benefited greatly from talking with the comfort coach. From simple distraction, things like a glitter wand to guided imagery…thinking about the beach, really helped during a time when I was in pain and being poked and prodded.” Another shared, “sometimes after a major surgery…you feel like a pin cushion, and you start to hurt. Being introduced to these techniques and the comfort coach had a calming influence on me.”
The CCLS was able to individualize interventions by providing adult coloring books, crossword puzzles, virtual reality, and other activities the patients requested, further strengthening the individualized interventions component. “The virtual reality goggles transported me from my chest pain.” Noting the benefit of techniques to transitioning home, a study group participant commented, “I have been using the meditation app and the glitter wand at home and at work. The techniques are proven to me, and I would highly recommend them and this service to others.” Two study group participants felt that because of the business of the inpatient unit, the timing of the CCLS-RT presence and interventions was “a little off.” This may have been due to the CCLS-RT covering a pediatric unit and supporting the research on an on-call basis rather than immediately available onsite in the cardiovascular center.
Participants’ perceptions of the role and value of the CCLS-RT in their care, as well as the overall participant experience, was also explored by the research team. Those who participated in the pilot program identified positive gains from their experience, “this provided support for me before, during and after my care…I even used the tools at home to help with my fears and pain following surgery.” Another patient commented that while the focus was on him during the intervention sessions, “my family benefitted from this service in addition to me.” Specifically addressing the overall research participation, a patient reported on the service provided, “this (support service) is something that helps patients and families to learn how to navigate the healthcare setting, it really helped me.”
Another study patient receiving comfort coach interventions shared, “The medications are regimented (as part of the patient care plan), and I could tell when I needed the next dose of medication right up to the minute. In that hour of discomfort until the next dose kicked in, the calming influence of the comfort coach was helpful to distract me and alleviate the pain.” Conversely, a control group participant stated, “relaxation or distraction techniques would have been helpful about 24 hours after surgery, at extubation, and during times of pain.”
The interview and telephone survey responses from the CCLS-RT, ACSCT, and the participants supported the concept of CCLS-RT integration into the ACSCT to provide meaningful interventions for improvement of the cardiac perioperative patient experience. Staff and providers indicated interest in the CCLS-RT role and its benefit to the interdisciplinary care team. The interviews demonstrated that the CCLS-RT specifically added value to the team and patient experience through utilization of non-pharmacologic techniques that were adapted for an adult patient undergoing cardiac surgery.
Study Changes
As a result of patient feedback from the pilot study, the survey process and the use of the iPad were eliminated for the subsequent larger scientific clinical trial. Patients commented that the iPad was challenging to use for a survey completion due to the sensitive touchscreen on the device. Patients also discussed the length of surveys and suggested a decrease in the number of screening surveys. The study team also decreased the number of initial screening survey questions from 80 to 30 questions for the larger clinical trial. Additionally, the original total of 320 questions over four surveys was reduced to 161 total questions across the four survey touchpoints. In the words of one participant, “I liked knowing someone else was there to help me through the experience that can help reduce anxiety and discomfort. It is comforting to know.”
Discussion
With the conception of child life originating 100 years ago, pediatric health care settings have greatly benefited from the child life specialist role, yet a similar comprehensive care role does not exist in adult care settings despite recurrent issues for adults with pain management, anxiety, and coping. Child life specialists connect with patients, meet patients where they are, help them understand, and provide comfort and support while cultivating resilience (Wolf, 2018). Could this be a multidisciplinary role within a hospital system? Potentially. Child life is uniquely qualified and poised to do this work. Other multidisciplinary support specialties would require substantial education and training to acquire the basic tools to function in this role. Child life specialists have the foundational knowledge, tools, skills, and abilities to capitalize on this opportunity to further make their mark on health care and to continue to evolve as a profession.
This pilot study was developed for several reasons, the primary being 1) an increased need for pain management support with adult patients, 2) an institutional priority to reduce the use of opioids for surgical patients, and 3) continued requests in the adult hospital for non-pharmacologic interventions and child life services support. Based on survey results and interviews with both study participants and staff, this pilot study appeared to indicate that the inclusion of a CCLS on the ACSCT team is not only feasible, but also appeared to be accepted and valued by all staff and patient stakeholder groups. Additionally, given the challenges and areas for improvement identified by these groups, it appears that such a program would be best accomplished with a dedicated, full-time CCLS, and an experienced research coordinator for the purposes of a larger clinical trial to assess outcomes. Many of the control group and experimental group patients in this pilot program indicated they appreciated the opportunity to participate in this program as a demonstration of the hospital’s commitment to their overall patient experience.
Perhaps, then, the foundations of child life knowledge and skills—their educational backgrounds, theoretical frameworks, and scope of practice—provide a strong foundation for child life specialists to provide individualized care feasibly and effectively to adult patients undergoing cardiac surgery (Pillai, 2020; Wolf, 2018). Furthermore, although a novel application of child life practice into a traditional adult healthcare setting, this pilot program appeared to be both feasible within logistical limits related to staffing, materials, and collaboration, as well as positively perceived by program participants and staff.
Limitations
Like any study, there were limitations to this work. First, this study intended to serve as a pilot precursor to an eventual randomized clinical trial; thus, there was limited funding, a small sample size, use of internally developed measures versus validated ones, and a lack of audio transcription from the post-intervention phone interviews. Additionally, this unfunded pilot study was staffed by professionals with competing clinical and administrative responsibilities and part-time research staff. As such, data collection points were occasionally missed because of part-time research staff availability and gaps in communication with the inpatient care team. Future work will include full-time, on-call research and clinical staff to improve and expedite data collection in the context of a randomized controlled trial design.
Conclusion
This pilot study applied the skills and experience of CCLS to deliver evidence-based non-pharmacologic interventions to adult cardiac surgery patients to improve non-pharmacological pain control options for this population. The results of this pilot study showed that CCLS role could be feasibly adapted and integrated into the adult clinical cardiac setting. In addition, the intervention was found to be accepted and valued by patients, families, and other members of the care team. The incorporation of the child life specialist into the adult cardiac clinical care team was acknowledged through surveys and interviews with patients, families, and care team members as a needed and positive contribution to patient experience with improvement in pain and anxiety.
Stepping into the adult world comes with significant and thoughtful consideration, with more work to be done to expand CCLS education, training, and supportive resources in adult patient care. As a pilot study, this work has contributed knowledge and experience within the bounds of scientific inquiry to explore the possibilities for adult-oriented child life care and next steps for research and practice. By engaging an array of multidisciplinary stakeholders, including cardiac surgery, nursing, advanced practice providers, social work, psychiatry, music therapy, art therapy, patients, families, and the Office of Patient Experience, this pilot program garnered buy-in from multiple groups and generated useful tools and practices to be adapted into a larger clinical trial. This expanded scientific research trial will provide the opportunity to objectively evaluate the impact of dedicated non-pharmacologic interventions facilitated by child life specialists on pain, anxiety, opioid use, health care resource utilization and patient experience in adult patients undergoing cardiac surgery.
Acknowledgment
Acknowledge with gratitude the department of Child & Family Life and particularly: Beth Karl, CCLS; Jessica Oswald, CCLS, Stephanie Sproles-Gooch, CCLS, Kimberly Manasco, CCLS who were our brave specialists initiating this work and Jessica Jenkins, CCLS who is carrying it forward.
Abbreviations
- CCLS – Certified Child Life Specialist
- CCLS-RT – Certified Child Life Specialist Research Team = “Comfort Coach” study terminology
- ACSCT – Adult Cardiac Surgical Care Team
- AF – Atrial Fibrillation
We utilized the term “comfort coach” for our CCLS-RT study terminology to avoid potential confusion for patients and adult care staff in the cardiovascular center, due to the well-known presence of child life specialist services in the children’s hospital. For ease of the reader, we will refer to CCLS-RT instead of using the comfort coach term unless listed on specific appendices.