In the United States, the most prevalent pediatric cancer diagnosis is acute leukemia, with acute lymphoblastic leukemia (ALL) as the most common subtype (Siegel et al., 2023). The treatment for ALL is usually two to three years of chemotherapy, requiring intravenous access weekly or monthly. Most patients with ALL have an Infusaport placed, a central venous line accessed using a needle. This can be a distressing activity for children with ALL, as repeated exposure to invasive medical procedures has been identified as a significant contributor to increased distress for pediatric patients (Rennick et al., 2004; Saylor et al., 1987). Research has found that children’s distress during pediatric cancer treatment has been associated with negative long-term outcomes (Kunin-Batson et al., 2014; Linder & Hooke, 2019; Pate et al., 1996). Specifically, persistent sadness, pain, and anxious and depressive symptoms early in treatment have been attributed to long-term difficulties in emotional functioning as well as more negative attitudes and healthcare avoidance behaviors beyond the completion of treatment and into adulthood (Kunin-Batson et al., 2014; Linder & Hooke, 2019; Pate et al., 1996). Therefore, psychosocial interventions that address children’s procedural distress early in treatment have the potential to positively impact long-term emotional functioning.
While there have been mixed findings regarding the presence of a habituation effect to invasive medical procedures (Dahlquist et al., 1986; Jay et al., 1983; Katz et al., 1980), more recent studies have not identified a habituation effect (Caes et al., 2014; Hockenberry et al., 2011; McMurtry, 2013; McMurtry et al., 2015; Sørensen et al., 2021), suggesting that repeated exposure to a medical procedure may not be sufficient to reduce distress. Additionally, memories of past procedural pain have been shown to impact subsequent procedural distress and coping, whereby children who recall more pain during a previous medical procedure demonstrate higher distress and more difficulty coping (Von Baeyer et al., 2004). Furthermore, children’s delayed recall of procedural pain is greater than pain reported immediately following the procedure (Cohen et al., 2001). Together, this indicates that children undergoing repeated, potentially painful medical procedures may be at higher risk of difficulties coping with repeated medical procedures.
Interdisciplinary psychosocial teams are well integrated into pediatric cancer care at many major medical institutions in the United States (Hord et al., 2014) and provide focused interventions targeting coping, adjustment to disease and treatment, and family functioning. Certified child life specialists (CCLSs) are valuable members of the interdisciplinary psychosocial team (Hord et al., 2014; Romito et al., 2021) with formal clinical training on the developmental impact of illness and use of evidence-based techniques to promote coping, decrease stress, and reduce anxiety during healthcare experiences (Fraser et al., 2019; Romito et al., 2021). CCLSs are often responsible for providing interventions surrounding invasive medical procedures (Armington et al., 2016; Brown et al., 2021; Fraser et al., 2019; Romito et al., 2021). Previous research shows CCLS-facilitated procedural support interventions have been helpful for children undergoing necessary procedures for a variety of medical conditions, including pediatric cancer (Baughn et al., 2022; Durand et al., 2015; Grissom et al., 2016; Hsiao et al., 2019; Waters & Dickens, 2021).
Children undergoing medical care who receive procedural support provided by CCLSs have significantly lower levels of anxiety, exhibit less distress and fear, demonstrate increased cooperative behaviors, and have better long-term coping and adjustment to future medical stressors, including subsequent procedures and hospitalizations (Claridge et al., 2020; Fraser et al., 2019; Romito et al., 2021). A recent systematic review examined the evidence of four common procedural support interventions (i.e., building coping strategies, medical play, preparation, and procedural support) and found that overall, most studies reported positive outcomes (e.g., reduced pain, distress, and fear) for children who received these psychosocial interventions, either separately or combined (Chrisler et al., 2021). This review demonstrates that research frequently examines interventions independently, and only one study was identified that investigated all four types of interventions in combination (Tyson et al., 2014). Although CCLSs are often primary team members providing procedural support (Romito et al., 2021), there are a limited number of studies examining interventions delivered by CCLSs (Chrisler et al., 2021). To the best of our knowledge, no studies to date have examined procedural support interventions delivered by CCLSs longitudinally.
Overall, the psychosocial burdens of pediatric cancer treatment as well as short- and long-term effects of distressing and painful medical procedures highlights the need for additional research on comprehensive procedural support. The current study aims to integrate all four psychosocial interventions surrounding medical procedures (i.e., building coping strategies, medical play, preparation, and procedural support) into a comprehensive intervention delivered serially by CCLSs, and evaluate children’s distress, pain ratings, and mood during Infusaport accesses for newly diagnosed patients with ALL.
Method
Participants & Procedure
Children diagnosed with ALL with planned placement of an Infusaport central line who were between two and 12 years of age were eligible to participate. Institutional review board approval was obtained. Prior to study enrollment, caregivers provided written consent and children provided verbal assent.
This study was conducted at a large academic medical center in the Mid-Atlantic region of the United States between 2018 and 2021. Families were recruited by study team members in the pediatric oncology clinic and inpatient unit during planned treatment visits. Study enrollment occurred before the child’s first Infusaport access, typically at the start of the consolidation phase of treatment (approximately one month after diagnosis), as the institutional standard is to place the Infusaport at the conclusion of induction.
Data were collected from participants across 15 timepoints including each of the child’s first 10 Infusaport accesses and five follow-up timepoints. Every child received comprehensive procedural support provided by a CCLS for all 10 Infusaport accesses. The first 10 timepoints were referred to as the primary intervention period. The average length of time for the primary intervention period was 68.62 days (SD = 19.31). Data were also collected at predetermined follow-up intervals two weeks, one month, three months, six months, and 12 months following the child’s 10th Infusaport access. These five timepoints were referred to as the follow-up period. The aim of the intervention was to scaffold the child’s independent utilization of skills to decrease distress behaviors and successfully cope with the Infusaport access procedure without CCLS intervention. During the follow-up period, comprehensive procedural support was only continued as needed per the assessment of a CCLS.
Prior to the start of each Infusaport access, the child was asked to rate their mood. Children were shown the mood measure, prompted with “How do you feel today?” and all anchors (e.g., “very happy,” “a little sad”) were read aloud prior to obtaining the child’s response. Video cameras (one stationary and one wearable head camera worn by the nurse) captured each procedure for later video coding. Following the completion of each Infusaport access, the child was shown the FACES measure, prompted with, “What did you feel during your port access today?” and asked to rate their pain. Again, all scale anchors (e.g., “hurts little bit,” “hurts whole lot”) were read aloud prior to obtaining the child’s response. This same procedure was followed for each of the Infusaport access procedures during the primary intervention and follow-up period. At the conclusion of the 10th Infusaport access, the child and caregiver were compensated with one $25 gift card for their participation.
Procedural Support Intervention
Procedural support interventions were predominantly delivered by the primary CCLS in the outpatient oncology clinic. However, five additional CCLS were trained on the study procedure and delivered the intervention if the primary CCLS was not available. All efforts were made to minimize the number of CCLSs that worked with each child to increase CCLS familiarity with the child’s preferences and coping plan.
Children were provided with pharmacological pain management via topical numbing cream (e.g., EMLA and LMX). Application of topical numbing cream was confirmed via video data for 206 of the 208 primary intervention port access procedures. Video data confirmed that one child did not receive topical numbing cream for one port access. The other video could not confirm the application of topical numbing cream, as the recording began after the child’s port was exposed. Overall, application of topical numbing cream was confirmed for 97.35% of the port access procedures included in this study.
This institution utilizes a primary nursing model, whereby every child is assigned primary outpatient and inpatient nurses at diagnosis. Therefore, there was considerable consistency in nursing care for each child across study procedures. This also allowed for close and ongoing collaboration regarding the child’s individual coping plan between the nurse and the CCLS. It was typical for the nurse and CCLS to engage in discussions regarding strategies to best support the child’s coping while safely and efficiently completing the port access both before and after each procedure. Discussions often included a review of the child’s specific stressors and individual coping plan, including specific strategies the CCLS was rehearsing with the child during the preparation phase of the intervention. This also allowed for open communication regarding specific behaviors that impeded the nurse’s ability to perform the port access. Reduction of these behaviors became additional targets for the intervention. Certain choices provided to the child, such as the positioning of their body, were only offered following the nurse’s physical examination of the port site to determine what was medically feasible. These examples only account for some of the collaborative efforts between the nurse and CCLS. Throughout each procedure, the nurse and CCLS supported each other’s roles and responsibilities and prioritized the needs of the child and caregiver.
Each intervention was individualized, accounting for the developmental level, temperament, and coping style of each child. Common components were implemented across every intervention in three distinct phases: 1) preparation; 2) support; and 3) reflection and included the integration of four types of interventions (i.e., building coping strategies, medical play, preparation, and procedural support).
Preparation prior to the start of the Infusaport access included education on the function of the Infusaport device, review of procedural steps, the child’s sensory experiences (e.g., what the child would feel, smell, and taste), setting role expectations for the child and caregiver, reviewing choices and preferences of the child, and the teaching and rehearsal of coping strategies, such as distraction and diaphragmatic breathing. It also included a discussion about the child’s past procedural stressors and collaborative problem-solving to proactively address anticipated stressors. A formalized plan based on the preparation listed above was outlined and referred to as the child’s coping plan. The preparation phase took approximately 30 minutes prior to the first Infusaport access. Subsequent sessions of preparation were often shorter, but always included a collaborative discussion about the child’s coping plan, stressors, and an assessment of the child’s recall of the procedural steps and their role (i.e., “jobs”).
During the preparation phase, medical play was facilitated at least once for every child. Most medical play sessions occurred prior to the first Infusaport access, and every child participated in medical play prior to their third Infusaport access. Children were provided with a combination of real and pretend medical equipment and a cloth doll with a mock Infusaport. A developmentally appropriate prompt (e.g., “you get to pretend to be the nurse and access the doll’s port” or “kids tell us they like to fit the pieces together to understand how their port works”) encouraged the child’s engagement. Medical play allowed the child to control and manipulate medical equipment, explore the sensory experiences of the materials, rehearse coping strategies, and provided an opportunity for the CCLS to address misconceptions about the steps and rationale for the procedure. CCLS-led medical play has been shown to be an effective preparation technique (Boles et al., 2020; Cuzzocrea et al., 2013; Jones et al., 2021).
The support phase of the intervention occurred during the procedure. This included the implementation of the child’s coping plan through various means, including verbal prompts reminding the child, caregiver, and nurse of their plan, continued assessment for specific stressors, providing additional developmentally appropriate information, and/or implementing behavioral strategies. An example of an 8-year-old child’s recollection of her individualized coping plan is depicted in Figure 1.
The final phase of the comprehensive procedural support intervention was reflection. Following the completion of the procedure, the child was asked what parts of their coping plan were helpful and what, if anything, should be revised for next time. Questions were posed to the child with the aim of differentiating the child’s perception of fear and pain. If the CCLS observed a particular stressor that increased distress during the procedure, this was brought to the child’s attention, and problem-solving was initiated around how to decrease distress during future procedures. While the questions were directed at the child, the discussion often included the child’s caregiver and nurse. Reflection discussions were documented and incorporated into the preparation phase of the following Infusaport access.
Measures
Demographic Characteristics
Caregiver and child demographic information were collected including the child’s date of birth, diagnosis, treatment information, ethnicity, relation of caregiver, marital status of caregiver, and household income. All demographic information was provided by the caregiver.
Brief Behavioral Distress Scale (BBDS)
The BBDS (Tucker et al., 2001) was designed to assess the child’s procedure-related distress. Each distress behavior observed during the medical procedure was coded as non-interfering (e.g., saying “ouch”), potentially interfering (e.g., screaming), or interfering (e.g., getting up from their seat). Behaviors were documented for each step of the procedure (e.g., cleaning skin and needle insertion). Higher total distress scores reflected greater child distress. The measure has previously been validated with Infusaport access procedures in pediatric oncology (Tucker et al., 2001). All procedures were video recorded and later coded. Chorney and colleagues’ (2014) practical guide to behavioral coding in pediatric psychology was used as a framework. To determine interrater reliability, two trained coders (i.e., MM and PP) reviewed a randomly selected subset totaling 25% of all recorded Infusaport access procedures. The interclass correlation coefficient, an established tool in determining interrater reliability (Koo & Li, 2016), was calculated, yielding excellent (r = .94) reliability for total distress scores.
Wong-Baker FACES Pain Rating Scale (FACES)
FACES (Wong & Baker, 1988) is a 10-point self-report measure utilized to assess the intensity of children’s pain. Item responses range from “no hurt” to “hurts worst” on a 10-point Likert scale. Pictures of animated faces were presented with each corresponding anchor to provide a concrete representation of no pain (0) to severe pain (10). This measure has been validated for children as young as 3 years of age for measuring pain associated with medical procedures (Wong & Baker, 1988).
Child Mood Rating (Mood)
Children rated their current mood on a 10-point Likert scale. This measure was adapted for this study by utilizing the animated faces on the FACES scale (Wong & Baker, 1988) and changing the anchors to “very happy” (0), “happy” (2), “a little happy” (4), “a little sad” (6), “sad” (8), and “very sad” (10). Higher scores indicated worse mood. Because this is a single-item measure, formal reliability analyses could not be conducted. However, the adaptation of this measure incorporated developmental theory. Extensive developmental literature suggests before three years of age children can identify and label basic emotions, including happiness and sadness, and the validity of such expressions are augmented when the child is provided facial expressions as cues (Durbin, 2010; Widen & Russell, 2008). While completing this measure, children easily and readily identified the emotions depicted. Although informally assessed, the CCLS noted congruence between the child’s chosen mood rating and observed behavior. On one occasion, a significant discrepancy between a child’s chosen mood rating and observed behavior was noted and excluded from analyses.
Data Analysis
Specific analyses were outlined to best evaluate serial comprehensive procedural support interventions on the child’s mood, total distress behaviors, and pain rating during Infusaport accesses at both the group and individual level. Because FACES has been validated for children three years of age and older, the two-year-old participant was not included in analyses involving mood and pain ratings. Additionally, children with more than five timepoints of missing data due to nonresponse were excluded from analyses involving that measure. Both SPSS and R statistical packages were used to complete all analyses.
Group level descriptive statistics were calculated for each of the 15 timepoints for children’s mood, total distress behaviors, and pain rating. Paired t-tests were calculated to examine if there were significant changes in mood, total distress behaviors, and pain rating at the group level over the course of the study timeline.
Clinically significant change statistics, such as the Reliable Change Index (RCI; Jacobson & Truax, 1991), shift the focus from group level change to an examination of the improvement or deterioration of individual participants (Morgan-Lopez et al., 2022) and provide a measure of statistical and clinical significance (Jacobson & Truax, 1991; Zahra & Hedge, 2010). Although variations on their original method have been proposed, the original formulation continues to be utilized by researchers as a well-established, psychometrically sound indicator of change (de Beurs et al., 2019; Vaganian et al., 2020). In this study, RCI scores were calculated for each participant to assess behavioral change across the primary intervention and follow-up periods.
Repeated measures correlations, to determine shared within-individual correlations for matched measures (Bakdash & Marusich, 2017), were calculated between total distress behaviors, pain rating, and mood using all timepoints in the study.
Results
Demographics
Twenty-five children were diagnosed with ALL during the enrollment period and were invited to participate. Twenty-one children and caregiver dyads (84%) agreed to participate. The caregivers’ relationship to their child included 15 (71%) mothers and 6 (29%) fathers.
The average age of the children at study enrollment was 7.30 years (SD = 3.24; range = 2.17 – 12.16 years). Eighteen (86%) of the children had pre-B acute lymphoblastic leukemia and three (14%) had T-cell leukemia. Twelve (57%) children were enrolled on Standard Risk and nine (43%) were enrolled on High-Risk treatment protocols. This sample was predominately White (n = 13; 62%) and non-Hispanic (n = 18; 86%). Median family income was between $51,000 and $99,999. A full breakdown of demographic information is provided in Table 1.
Throughout the course of the study, data was not collected during 12 port access procedures, representing 3.8% of all study port access procedures. Missing data occurred due to a number of medical and logistical reasons including port removal prior to the 12-month follow-up, transfer of care to a different institution, camera malfunctions, and delay in IRB approval of our continuing review during the COVID-19 pandemic. Three children were excluded from mood and pain analyses due to being less than three years old or missing more than five pain and mood responses. These three children were all two and three years of age and female. Of note, there were other three-year-old children who provided self-report data and were retained in the mood and pain analyses.
Procedural Distress
Descriptive Statistics and Distress Trajectory
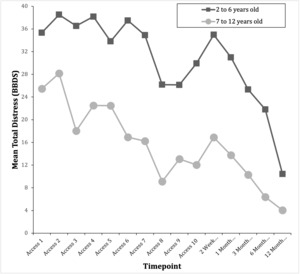
The average total procedural distress score for each timepoint across participants was plotted to show the trajectory of distress behaviors during the primary intervention and follow-up periods (Figure 2). Overall, the trajectory of distress behaviors appeared to be trending downward throughout the primary procedural support intervention and follow-up period. The mean and standard deviation of total distress scores for each timepoint is presented in Table 2.
Due to the distinct developmental abilities of children in this sample, separate average total distress scores for each timepoint were graphed for children ages two to six and seven to 12 years of age (Figure 3). Similar trajectories emerged, providing support that both age groups exhibited declining distress behaviors throughout the study.
Mean Differences
Due to the small sample size, longitudinal modeling could not be completed. Instead, early distress composite scores were calculated by averaging total distress scores for Infusaport access 1 and 2. Similarly, end of primary intervention distress scores were calculated by averaging total distress scores for Infusaport access 9 and 10. Paired t-tests were used to assess potential mean differences. Children demonstrated significantly less distress at the end of the primary intervention period (M = 19.93, SD = 21.17) and 12 month follow-up (M = 7.60, SD = 5.21) than their early Infusaport accesses, M = 31.64, SD = 24.86, t(20) = 2.99, p = .007 and t(17) = 4.78, p < .001, respectively. Additionally, children’s distress was significantly lower at the 12 month follow-up than at the end of the primary intervention, t(17) = 3.23, p = .005. Overall, these results reflect statistically significant reductions in distress behaviors during the primary intervention period and the follow-up period.
Clinically Significant Change in Distress Behaviors
RCI scores were calculated for all participants. RCI scores greater than +/-1.96 are statistically significant with p < .05. Positive RCI scores indicate improvement and negative RCI scores indicate behavioral deterioration. At the end of the primary intervention period, 14 out of 21 children (67%) showed statistically and clinically significant improvement with an RCI score greater than 1.96 (n = 9) or had a distress score of 0 for both their 9th and 10th Infusaport access procedures (n = 5). The mean RCI for all 21 children was 1.34 (SD = 2.06). One child demonstrated significant behavioral deterioration in distress (RCI = -2.09). This child had a delayed distress peak at access 8 due to a procedure requiring multiple needle insertions. This child’s RCI between access 8 and end of primary intervention distress did demonstrate significant improvement (RCI = 2.28). Fourteen out of 18 (78%) children showed clinically and statistically significant improvement from the beginning of the intervention to the 12-month follow-up as demonstrated by an RCI score greater than 1.96 (n = 11) or a distress score of 0 (n = 3). The mean RCI for all 18 children from the beginning of the intervention through the 12-month follow-up was 2.86 (SD = 2.54).
RCI scores were also calculated from the end of the primary intervention period through the 12-month follow-up. During this time, no child demonstrated significant behavioral deterioration. Every child who had achieved significant improvement maintained their reduction in distress behaviors over the next 12 months. From the end of the primary intervention period through the 12-month follow-up, one child demonstrated significant improvement who had not previously. Additionally, two children who had demonstrated significant improvement previously demonstrated another clinically and statistically significant reduction in distress behaviors.
In summary, 18 of 21 (86%) children enrolled in the study demonstrated a clinically and statistically significant reduction in distress behaviors during the study timeline. No child demonstrated a significant behavioral deterioration after demonstrating significant improvement, supporting maintenance of reduced distress behaviors. Three out of the total 21 children who enrolled in the study (14%) never met reliable change parameters.
Pain Rating Analyses
Descriptive Statistics and Pain Rating Trajectory
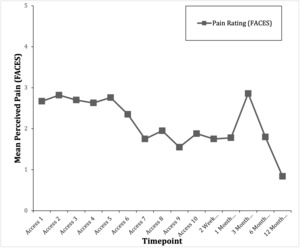
The average pain rating for each timepoint across participants was plotted to show the trajectory of perceived pain during the study (Figure 4). Overall, the trajectory displays a downward trend throughout the primary intervention. Post-intervention, there was some fluctuation in pain rating and was lowest at the 12-month follow-up (M = 1.00, SD = .97). Mean and standard deviation for pain rating at each timepoint is in Table 2.
Mean Differences
Composite early (mean pain for access 1 and 2) and end of primary intervention (mean pain for access 9 and 10) pain rating scores were calculated. Paired t-tests assessed for potential mean differences in pain rating. Children’s pain rating during early Infusaport accesses (M = 2.94, SD = 2.53) was not statistically different from their pain rating at the end of the primary intervention period, M = 1.76, SD = 2.10, t(17) = 1.89, p = 0.08. Children reported significantly less pain at the 12-month follow-up, M = 0.84, SD = 0.96, than during their early Infusaport accesses, t(15) = 3.25, p = .005. Additionally, the difference between pain rating at the 12-month follow-up was significantly lower than pain rating at the end of the intervention period, t(17) = 2.19, p = .04. Children’s pain rating was significantly lower at the 12-month follow-up than during early or end of primary intervention Infusaport access procedures.
Mood
Descriptive Statistics and Mood Trajectory
The average mood for each timepoint across participants was plotted to show the trajectory of mood during the primary intervention and follow-up periods (Figure 5). Overall, there is not a clear trend with fluctuations in mood throughout the primary intervention and follow-up periods. Due to no clear trend in mood, further analyses were not conducted. Mean and standard deviation for mood at each timepoint is listed in Table 2.
Repeated Measures Correlations
There was a significant, positive repeated measures correlation between total distress behaviors and pain rating, r(234) = .218, p < .001, 95% CI [0.09, 0.33]. More distress behaviors were associated with greater pain rating in individuals. There was a significant, positive correlation between mood and total distress behaviors, r(235) = .369, p < .001, 95% CI [.25, .47]. Higher mood scores, indicative of worse mood, were associated with more distress behaviors in individuals. There was a significant, positive correlation between mood and pain rating, r(233) = .168, p = .010, 95% CI [.04, .29]. Higher mood scores, indicative of worse mood, were associated with greater pain rating in individuals.
Discussion
This pilot study examined distress behaviors, pain rating, and mood during children’s Infusaport access procedures while receiving comprehensive procedural support provided by a CCLS. Results showed the majority of children demonstrated a statistically and clinically significant reduction in distress behaviors across time. No child demonstrated significant behavioral deterioration after demonstrating significant improvement. Additionally, children’s pain ratings were significantly lower at the 12-month follow-up than the early or end of primary intervention Infusaport access procedures. Overall, the findings of this study are in line with previous studies which found that procedural preparation and support may decrease distress behaviors and pain rating (Getchell et al., 2022; Jones et al., 2021; Sanchez Cristal et al., 2018).
The further decrease in distress and pain following the primary intervention period may be due to continued comprehensive procedural support interventions for children who exhibited ongoing behavioral distress at the end of the primary intervention period. Discontinuation of the comprehensive procedural support intervention was determined by the clinical judgement of the CCLS. Following discontinuation of the comprehensive procedural support intervention, nurses reported notable increased distress behaviors to the CCLS, allowing for subsequent support to be provided as needed.
Notably, we also found that, at the individual-level, distress behaviors, pain rating, and mood were all significantly correlated within participants across time. Worse mood was associated with more distress behaviors and greater pain rating and more distress behaviors were associated with greater pain rating. However, unlike distress and pain, average mood examined at the group level did not clearly trend up or down throughout the intervention and follow-up periods. Previous research has demonstrated that providing information about medical experiences can improve mood between initiation and conclusion of information provision and that improved mood extends to the conclusion of a single healthcare encounter (Burns-Nader et al., 2013). Our study recorded one mood rating prior to each port access across multiple, repeated procedures and, therefore, could not have captured changes in mood across each procedure, making it difficult to compare results across studies. Due to the proximity of our measurement of mood to the child’s port access procedure, the mood rating may be indicative of the child’s stress appraisal. Multiple theoretical frameworks delineating coping outline the central role of an initial emotional response and describe effortful processes and skill development that overrides these more automatic emotional responses to produce behavior change (Compas, 1987; Skinner & Zimmer-Gembeck, 2007). It may be that the relatively stable mood ratings in our study reflect a continued perception of the port access procedure as a stressful event. However, as children increase their coping skills, they are able to override their initial emotional response and facilitate more stable behavior change over time.
Multiple components of the intervention may have reduced the child’s distress behaviors and pain rating, particularly increasing perceived control, increasing emotion regulation abilities, and reducing uncertainty. Previous studies demonstrated that procedural support is associated with increased sense of control (Boles, 2016; Mcgrath & De Veber, 1986), and increased sense of control has been linked to better adjustment outcomes (Nannis et al., 1982; Segers et al., 2022). Additionally, multiple components of our intervention aimed to improve the child’s emotion-regulation by utilizing multiple emotion regulation strategies, including situation modification (e.g., positive parental touch), attentional deployment (e.g., distraction techniques), cognitive change (e.g., reappraisal), and response modulation (e.g., deep breathing strategies; Gross, 2015). Emotion regulation skills are a well-known mechanism influencing overall adjustment that can be improved with practice across time (Moltrecht et al., 2021). Furthermore, illness uncertainty, which is the perception of healthcare related events as difficult to understand due to ambiguity, complexity, unpredictability, and lack of information, has been associated with difficulty coping with medical related stressors and decreased emotional functioning for children with chronic illnesses, including pediatric cancer (Fortier et al., 2013; Mishel, 1981; Szulczewski et al., 2017). By providing children with the rationale for the port access procedure, sensory experiences, specific procedural steps, engagement in medical play, as well as the rehearsal and consistent implementation of an individual coping plan, this intervention may have reduced their overall uncertainty and increased their successful implementation of coping strategies to reduce distress. Further investigation is needed to identify the potential underlying mechanisms of these results.
A strength of the current study is that it was designed so that no child experienced an Infusaport access procedure before enrolling in the study. As such, there may be a preventative component inherent in this design to reduce negative experiences beginning with the first port access procedure. The importance of intervening as early as possible is supported by research examining the role of classical conditioning and expectancies in children’s pain, whereby children who received pain reduction interventions from their initial painful experience demonstrated less subsequent pain, even after pain reduction interventions were no longer provided (Gniß et al., 2020). While it is an inevitability that these children experienced other invasive and potentially painful medical procedures prior to their first port access and the extent of procedural support received prior to enrollment on study is not known, our study design prioritized providing maximum support from their initial port access and may have contributed to successful reductions in distress and pain ratings. While further research is needed, early implementation may optimize the impact of procedural support interventions on repeated medical procedures.
It is important that all members of the interdisciplinary medical team are aware of evidence-based procedural support strategies to advocate for appropriate delivery of interventions. CCLSs have formalized training in providing procedural preparation and support that makes them ideal members of the interdisciplinary team to deliver interventions of this kind in strong collaboration with nurses completing the port access procedures. As shown in previous research, the strategies outlined in this intervention have been implemented by a variety of interdisciplinary medical team members with appropriate training to help reduce children’s distress behaviors and pain rating.
Limitations
This study has several limitations, including limited sample diversity. Our sample was predominately comprised of White and middle-class children and caregivers, which may reduce the generalizability of the results and underscores the need for larger, more diverse samples to further investigate if similar associations are generalizable across various identities and in the context of other social determinants. Mood and pain ratings were prompted by the CCLS who provided the intervention, and therefore, may have been influenced by demand characteristics. Additionally, the mood measure was adapted for this study and, although informed by developmental theory, no formal analyses of validity and reliability were conducted. Therefore, it is possible that this measure is not assessing the desired construct of mood. Furthermore, most of the interventions were delivered by the same CCLS, which may have produced specific interventionist effects that are not accounted for within these results. This study has limited power due to the small sample size and lack of a control group. Due to the well-integrated nature of child life services prior to initiation of the study procedure, it would have been unethical to withhold standard psychosocial care from some participants to better delineate the causal effects of the intervention. Additionally, institutional funding and staffing resources limited the ability to employ a more complex experimental design. As such, the results of this study are strictly correlational, and time and exposure may have confounded the results of this study. Future studies utilizing experimental designs are needed to tease apart if these results are due to the comprehensive procedural support intervention rather than exposure or habituation.